On your way to Biology mastery? Enrol in our 99.5 studyscore masterclass. Click here!
Inquiry Question 3: How does the human immune system respond to exposure to a pathogen?
Content Descriptor: Investigate and model the innate and adaptive immune systems in the human body: (7.3.1)
1st line of defence:
Physical and chemical barriers which prevent the entry of pathogens to the body and make an inhospitable environment for foreign pathogens. The first line of defence is passive.
Skin:
- Thicklayer of keratin protein prevents penetration
- Drynessprevents growth
- Glandssecrete anti-fungal chemicals
- Overcome through cuts, abrasions or burnsMucous membranes:
Mucous membranes:
- Coveringdigestive and respiratory tracts
- Trapspathogens so they can be removed by cilia, coughing or sneezing
- Overcome through resistant sporesCilia:
- Small hair like structures which occur in large numbers on the cell surface, used forlocomotion
- Beatlike a series of oars, sweeping mucous
- Can be by-passed by avoiding them, infection of the upper respiratory tractOther secretions and chemical barriers:
- Gastricjuices destroy enzymes of pathogens
- Urineis acidic, inhibiting the growth of bacteria
- Resistantspores and antibiotics which disturb pH levels may weaken this barrier
2nd line of defence:
Once successful in penetrating the first line of defence, pathogens must now face the second line of defence. This is non-specific and attempts to destroy any pathogens present before they can cause any serious damage to the body. The mechanisms, or defence adaptations; cell death, inflammation, phagocytosis and lymph activities.
- Cellis injured by trauma or infection causing release of
- Histamine and other chemicals cause vasodilation and increased permeability of blood
- Increasedblood flow and increased permeability causes
- White blood cells enter tissues, triggered by increased blood flow and chemical signals.These include phagocytes such as macrophages which can engulf and digest foreign Pus is a bi-product of the clean-up process, composed of dead tissue, pathogens and white blood cells, as well as fluid from the capillaries.
- Neutrophils – First to move to the infection site, working to fight short and acuteinfections, self-destruct after a few days.
- Macrophages – The largest phagocyte, long lasting. Fighting chronic infections.After having engulfed an antigen, they release enzymes to destroy the particles then display the antigen on the MHC II molecule on the surface of the cell, this plays a vital role in the initiation of the third line of defence.
- Cell death – Cells die to seal off a pathogen that is not being successfully defended by thebody (granulomas). A wall of dead cells is made, forming a capsule trapping the pathogens inside. The debris is then destroyed by macrophages. These are common in chronic
- Lymph system – Lymph system involves the movement of lymph fluid around the body.It is a one-way drainage system, that has no pump and relies upon locomotion of adjacent muscles to operate. As well as housing B cells and T cells, they also house stationary When plasma from lymph is exchanged with the blood, pathogens get caught up. These then get filtered through the lymph nodes, where they are destroyed by macrophages.
- Othersecretions:
- Interferons - Secreted by some cells when infected by viruses cause nearby cellsto produce anti-viral enzymes. Most effective in short term infections. Short acting and non-specific.
- Compliment system – A group of 20 proteins which stimulate phagocytes tobecome more active or destroy membrane of invading
3rd line of defence:
Third line of defence is a specific response to a pathogen, aiming to neutralise pathogen and the antigens through cell and antibody mediated immunity. Many of the interactions are dictated by chemicals such as cytokines (interleukin)
Antigens:
- Anythingwhich can stimulate an immune response
- MHC I molecules are found on almost all cells. These molecules are antigens but arerecognised as self-antigens
- MHCII molecules found on macrophages and B-cells
- Pathogenswhich enter the body are a source of non-self-antigens
- Failureto recognise self/non-self-antigens leads to auto-immune conditions
- Can range from microbes and their toxins to grain and pollenAntibodies:
- Alsocalled immunoglobulins are proteins made in response to antigens
- Through a variety of methods antibodies neutralise a specific antigenResponse:
- Antigen is identified. This is either through being recognised by B-cells present in thelymph nodes, or identified by macrophages, which present the
- Helper T-cells recognise this identification, releasing interleukin 2 to stimulate their ownmass-reproduction. These helper T-cells then release chemicals which activate cytotoxic T-cells and B
- The specific B-cell to the antigen identified is cloned rapidly and begin pumping outantibodies to neutralise the antigen. Cytotoxic T-cells migrate to the area and begin attacking and killing infected cells.
- Memory cells of both B and T cells are created. When the antigen is identified to thesecond time, these memory cells are far faster to respond, reacting so fast that sometimes symptoms do not even present. The advantage of these over regular cells is that memory T-cells do not require helper T-cells to stimulate them, and memory B-cells produce antibodies extremely
- Once the infection has been defeated, suppressor T-cells halt the immune responseB-cells:
- Maturein bone marrow
- Releasedinto the blood, lymph nodes, spleen and tonsils
- Whenactivated, differentiate into plasma cells which secrete antibodies
- Alsodifferentiate into memory B-cells
- Defend against extracellular pathogensCytotoxic T-cells:
- Maturein the thymus
- Whenactivated migrate to the site of the infection and destroy infected cells
- Defendagainst intracellular pathogens
Content Descriptor: Explain how the immune system responds after primary exposure to a pathogen, including innate and acquired immunity: (7.3.2)
Terminology:
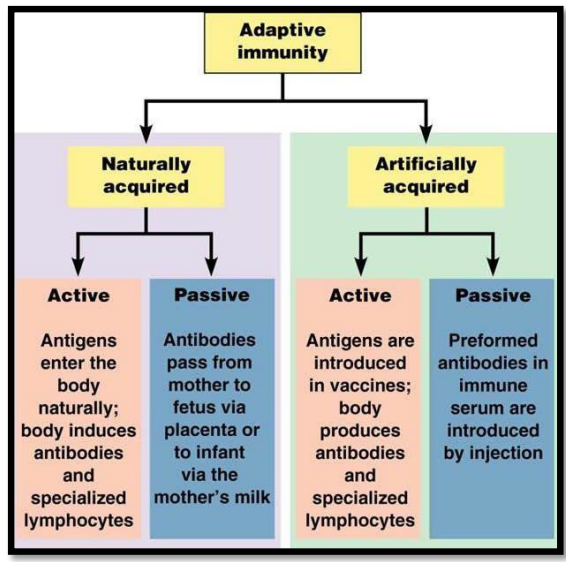
Acquired – Where the immunity is obtained from. This may be artificial (acquired through medical intervention) or natural (acquired through natural methods).
Innate – Innate immunity refers to the non-specific immune response, the 1st and 2nd lines of defence.
Active vs passive – Whether the body had to produce the antibodies itself. If the antibodies had to be produced by body cells, it is considered active. If the antibodies were injected, it is considered passive.
Exposure:
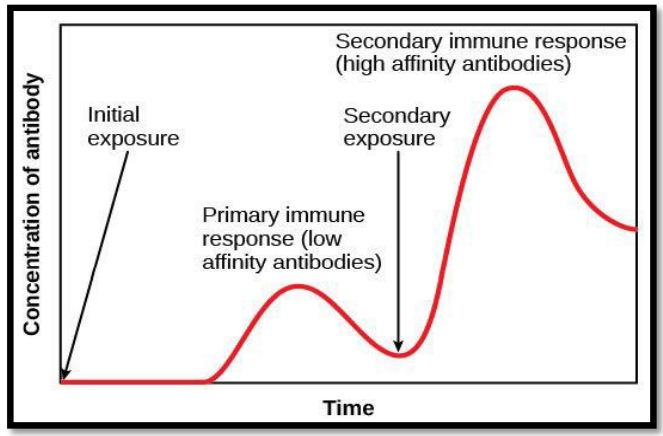
- Primaryexposure to an antigen is a very slow response, which can take up to a few weeks
- However, once the infection is fought, antibodies remain in the bloodstream for up to monthsafterwards, meaning no symptoms are even displayed when the antigen is encountered for the second
- Even if the level of antibodies falls beneath the minimum threshold, the later responses are also much faster due to the extremely fast replication of memory B and T-cells and produce much more antibodies. Later responses also require less antigen to initiate the response
Inquiry Question Review: How does the human immune system respond to exposure to a pathogen? (7.3.3)
You should be able to:
- Describethe innate and adaptive immune responses
- Describethe primary and secondary responses to pathogens
Inquiry Question 4: How can the spread of infectious disease be controlled?
Content Descriptor: Investigate and analyse the wide range of interrelated factors involved in limiting local, regional and global spread of a named infectious disease: (7.4.1)
Local Control Methods:
- Engaging with local communities through education awareness campaign about thesymptoms and associated risks
- Havinganti-bacterial gel at the entry and exit to buildings
- Reporting and isolation of individuals, such as the separation of confirmed cases fromsuspected cases in treatment centres
- Vaccinesare given to those who have been in contact with the infected
- Lowers risk of transferal from person to person, however is likely to breakdown if there is alack of trust between local authorities and locals
Regional Control Methods:
- Tracing anyone who was or has been in contact with the infected to ensure the disease is notspread to other areas
- Fasttargeted teams deployed to isolate the sick
- Medianotifications played a vital role in raising the alarm
- Isolationof villages via roads, to contain the sick and protect the healthy
- Can be a large drain on resources, technology may not be readily available to the developing world.
International Control Methods:
- Stockpilingof vaccines in the case of an international outbreak
- International monetaryand medical support
- WHOmay recommend restriction to international trade (pursuant to the IHR 2005)
- Quarantiningthose from west African nations if fever like symptoms are displayed
- Resourcesof international community are usually far better suited to tackle large issues
- Canbring a wide range of doctors with better training
- Intervention by the international community can lead to cultural misunderstandings which canbrew hostility